Translating evidence based research data to transform public health at scale
In a fast-paced digital age, ground-breaking research discoveries about innovative therapies, medtech advancements and new diagnostic capabilities for healthcare are announced every day.
These developments offer hope to patients, especially when living longer can present healthcare challenges, such as increased incidence of chronic diseases, diabetes, cancer, high blood pressure, high cholesterol, and heart disease.
Delivering value-based care and outcomes
As these advancements become available, healthcare systems around the world now face a new era of decision-making: How can healthcare providers utilise these cutting-edge innovations in a way that will still deliver value-based care and outcomes?
To support effective healthcare decision-making, there is a community of professionals highly skilled in using sophisticated analytical tools to crunch through large-scale datasets, unpack data and generate useful insights. This area of expertise is known as Health Economics and Outcomes Research (HEOR), and it is a relatively new area that has emerged more prominently over the past few years.
Today, HEOR has the potential for far-reaching positive impact on public health especially as healthcare systems continue to seek ways to stay sustainable for the future.
HEOR not only assesses the affordability and sustainability of health expenditure, but also draws links between treatment and actual outcomes in research patient cohorts to ensure evidence-based guidance on how to improve care at scale.
HEOR efforts in diabetes care
On this front, the Singapore Clinical Research Institute (SCRI) has a team of Epidemiologists passionate about HEOR and who have been supporting research projects in areas such as diabetics management, primary care and health technology assessment (HTA), among others.
To mark World Diabetes Day, we spotlight two research projects that SCRI’s HEOR team is collaborating with at the National Healthcare Group Pharmacy (NHGPh) and National Healthcare Group Polyclinics (NHGP).
Senior Epidemiologist Dr Yoko Wong is working on the first project that looks into a more accurate way to calculate and determine medication adherence among patients with Type 2 diabetes.
For the second project, Senior Epidemiologist Dr Guo Liang is studying the potential impact of weight reduction in reversing Type 2 diabetes.
Their sharp data analytic skills can help transform data gathered from fieldwork into ground-breaking insights that determine the impact of the research outcomes.
 Uncovering gems of data: Dr Guo Liang (Left), Senior Epidemiologist and Dr Yoko Wong (Right), Senior Epidemiologist at SCRI are passionate about Health Economics and Outcomes Research (HEOR). They are collaborating with National Healthcare Group Pharmacy (NHGPh) and National Healthcare Group Polyclinics (NHGP) on two research projects in diabetes management.
Uncovering gems of data: Dr Guo Liang (Left), Senior Epidemiologist and Dr Yoko Wong (Right), Senior Epidemiologist at SCRI are passionate about Health Economics and Outcomes Research (HEOR). They are collaborating with National Healthcare Group Pharmacy (NHGPh) and National Healthcare Group Polyclinics (NHGP) on two research projects in diabetes management.
Diabetes in Singapore
In Singapore, more than 400,000 people are living with diabetes, and of that number, 220,000 people are living with Type 2 diabetes [1].
Type 2 diabetes is often managed through medication to improve and regulate the blood sugar levels of a person with diabetes. However, about one in three living with diabetes are not adhering to their medication[2]. This can be attributed in part due to their doubts about the safety and efficacy of the medication, or them feeling well or having no visible signs of the disease.
Poor adherence to diabetes medication such as glucose-lowering drugs can result in poor control of blood sugar levels, increasing the risk of serious complications such as kidney failure, heart attack or stroke.
Medication adherence is thus a complex challenge for patients managing Type 2 diabetes. Key factors that determine medication adherence vary, ranging from patient education and practical methods such as setting reminders to take their medication.
Medication adherence study by National Healthcare Group Pharmacy / National Healthcare Group Polyclinics (supported by SCRI)
In this research study by lead investigator, Yap Hui Rei, Senior Pharmacist at NHGPh, retrospective research was done across five NHG polyclinics to study the medication adherence of 789 patients who were receiving regular care at these polyclinics.
The study gathered the data of anti-diabetes medication that was prescribed and dispensed to these patients from July 2016. The study continued to track the medication prescription and dispensing records till end of June 2017.
Calculating medication adherence
Proportion of Days covered (PDC) is a method used internationally to measure medication adherence from electronic medical records. PDC is used by healthcare teams, pharmacists and researchers to assess the quality of care and the clinical outcomes of patients. It is commonly calculated as a percentage by dividing the sum of days covered by medication over the designated measurement period. A common threshold for adequate adherence is if the patient consumed at least 80% of the medication supplied.
“Being able to identify sub-optimal medication adherence early and accurately will help medical teams, including doctors, pharmacists and diabetes care nurses identify patients at risk for treatment failure and provide early interventions,” said Hui Rei.
“Currently, there is no standardised approach to calculate and report PDC,” she added.
Together with her team of researchers, Hui Rei developed a series of new algorithm models to quantify medication adherence using prescribed and dispensed records to generate various scores of PDC. Next, the study sought to introduce an appropriate method for PDC calculation specifically tailored to the Singapore context. In this collaboration, Yoko further analysed the research data and translated the insights to support in-depth research.
 Type 2 diabetes is often managed with the use of medication to improve and regulate the blood sugar levels of a person with diabetes. A common threshold for medication adherence is if the patient consumed at least 80 per cent of the medication supplied.
Type 2 diabetes is often managed with the use of medication to improve and regulate the blood sugar levels of a person with diabetes. A common threshold for medication adherence is if the patient consumed at least 80 per cent of the medication supplied.
Valuable data mining
Yoko shared that data cleaning “can be tedious” because it involves trawling through volumes of data and identifying important ones for further analysis. Yet she derives “joy from the knowledge and understanding gained from studying the data, and how dealing with real world data can lead to more evidence-based findings to impact health outcomes of patients living with diabetes.”
For this project with Hui Rei, Yoko discovered that not all anti-diabetic medications are prescribed for the full duration of the measurement period, and suggested to the PI that this might be a significant factor to explore in her research. Yoko also highlighted that the pattern of dispensation and prescription in the Singapore context was different from other countries.
“In the polyclinics in Singapore, medication is subsidised so patients are more likely to collect all the medication prescribed and hence, the ratio between prescribed and dispensed medication is very close,” said Yoko, who holds a PhD in Genetic and Molecular Epidemiology (GAME) and a Master’s degree in Public Health.
After running comparisons on the data, Yoko was able to advise Hui Rei on the next steps of her research journey, for example, how the data can be interpreted or the various ways that the data can be further analysed and reported.
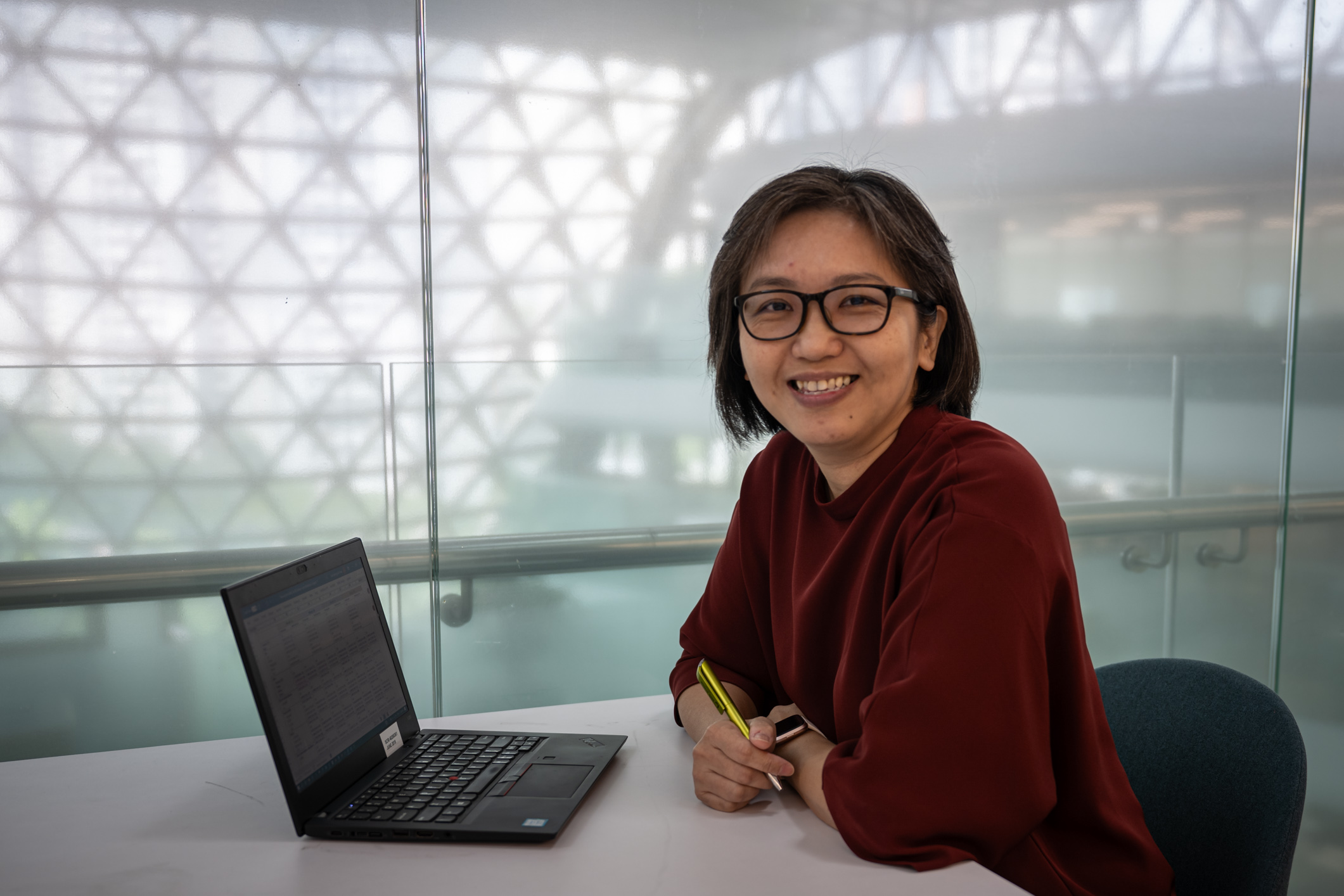 Dr Yoko Wong, Senior Epidemiologist at SCRI likens data crunching and analysis to going on a treasure hunt to uncover hidden insights from large-scale data
Dr Yoko Wong, Senior Epidemiologist at SCRI likens data crunching and analysis to going on a treasure hunt to uncover hidden insights from large-scale data
Data-driven insights
Through this study, the preliminary analysis showed promising results. This research would pave the way for further research to validate the assumptions for different PDC algorithms.
In the long run, it is hoped that such algorithms offer better accuracy for tracking medication adherence and patients can benefit from more timely interventions in managing their diabetes with sustained quality of life for many years to come.
Diabetes remission study by National Healthcare Group Polyclinics (supported by SCRI)
A diabetes remission clinical trial[3] led by NHGP aims to study the effectiveness of an intensive weight loss programme in achieving diabetes remission in obese patients with Type 2 diabetes.
The clinical trial, co-funded by the Tanoto Foundation and NHG Fund, began participant recruitment in early 2023 and is recruiting participants aged 21 to 60 with a body mass index (BMI) ranging from 27 to 45, and who have diabetes for less than six years and do not have further secondary complications caused by diabetes.
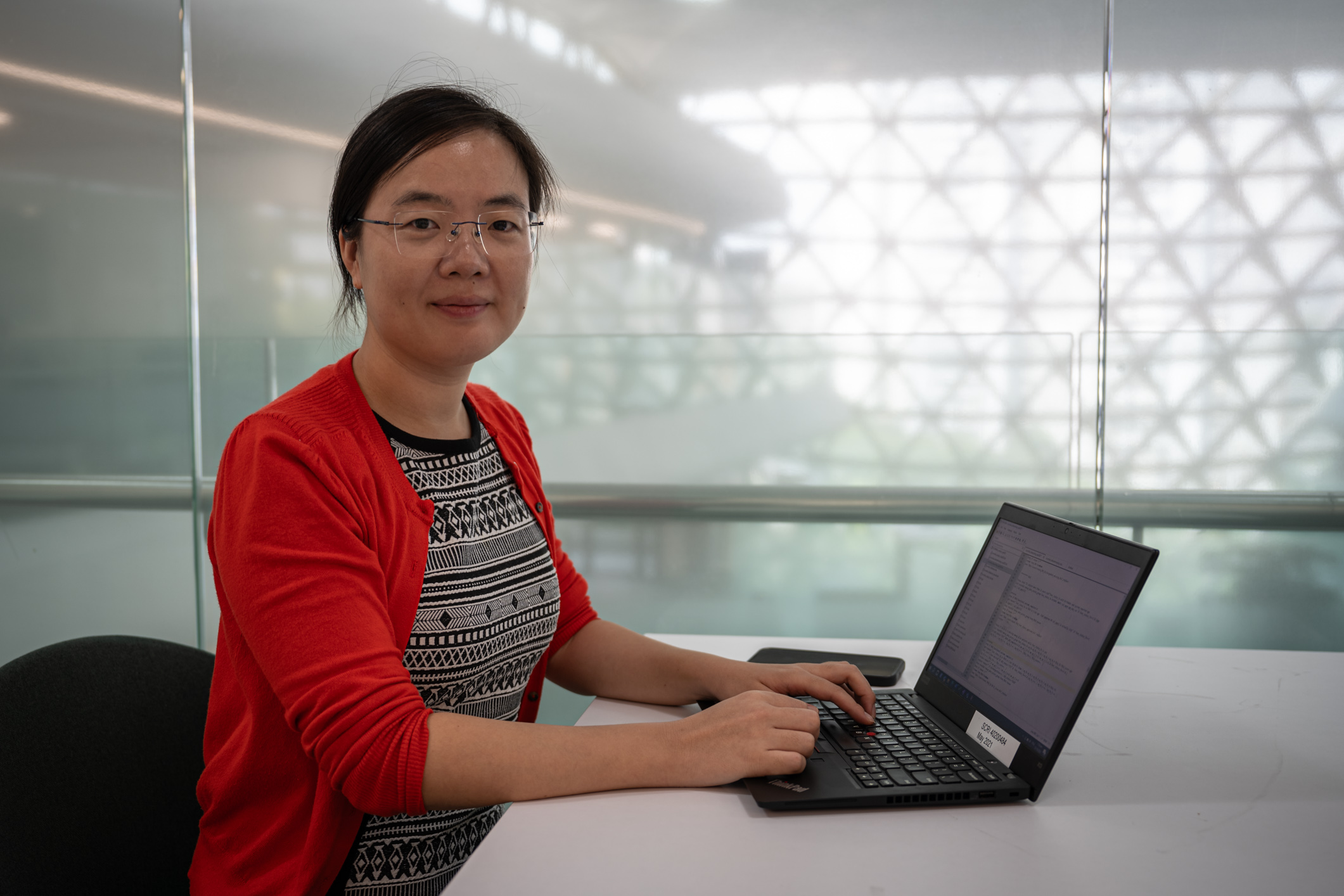 Dr Guo Liang, Senior Epidemiologist at SCRI shares that her role in research is like a data alchemist, turning raw research data into “research gold”. Together with her team, they guide researchers on how to run robust research studies that will return valuable insights
Dr Guo Liang, Senior Epidemiologist at SCRI shares that her role in research is like a data alchemist, turning raw research data into “research gold”. Together with her team, they guide researchers on how to run robust research studies that will return valuable insights
In this study, participants are randomly assigned into either control or intervention groups. The intervention involves a dietitian-led intensive weight management programme.
Guo Liang, Senior Epidemiologist at SCRI is working closely with the study’s lead investigator, Associate Professor Tang Wern Ee, Senior Consultant at NHGP and her team.
“The focus for this trial is to intervene early in patients with diabetes and to achieve diabetes remission through weight management instead of simply using medications to control their blood sugar levels,” said A/Prof Tang.
Studies have shown that even if diabetes remission is not achieved by significant weight loss in some individuals, there are still good health outcomes such as overall better control of blood sugar and blood pressure levels.
SCRI will be supporting this project from the early stages through to its completion in 2025.
 A research study at NHG Polyclinics is looking to see if diabetes remission can be achieved in study participants through significant weight loss over six months.
A research study at NHG Polyclinics is looking to see if diabetes remission can be achieved in study participants through significant weight loss over six months.
Strong foundations that drive data-driven research
Just like how a building requires a firm foundation to meet safety requirements, clinical research studies also require a strong foundation to ensure data integrity and validity.
According to both Yoko and Guo Liang, important considerations when embarking on a research study include thinking about the study design, selecting the right comparison group of patients, factoring in the study time frame, as well as reviewing if the outcomes from the research study adequately answers the research problem statement.
“Researchers will come to us with the research dataset collected from the field work and hope our analysis validates the data and supports their study findings,” said Guo Liang who holds a medical degree with specialisation in preventive medicine and a Master’s degree in Public Health.
“However, we usually educate our collaborators that different kinds of datasets, such as retrospective versus prospective dataset have different formats and each will produce different research insights,” she explained.
“Therefore, identifying the right variables to look at and clean the data judiciously can make all the difference,” she added.
Guo Liang also shared that when the study fieldwork is completed next year, she will verify the data for accuracy and thereafter, analyse the datasets and support the lead investigator in drafting the manuscript report.
Finding gold: Transforming data into valuable insights
In elaborating the important work she does, Guo Liang likens her role to a data alchemist who transforms raw research data into “research gold”.
“We have discussions with the principal investigators and advise them on the best practices for data collection, so that on our end, the data can be formatted and turned into meaningful insights using data analytics platforms like STATA,” she said.
She added on that insights from high-quality synthesised evidence research will in turn enable other stakeholders like PIs in their decision-making for improved health outcomes.
“Although analysing data takes time, ranging from weeks to months, when we are finally able to transform data into meaningful findings, it is rewarding,” said Guo Liang, who delights in “being able to indirectly find an effective intervention to help patients better manage and control their diabetes”.
Undoubtedly, diabetes-related research studies such as these provide valuable insights for medical teams to optimise patient care, introduce solutions for self-care, as well as sustain healthcare systems in managing this chronic condition in the population.
References
[1] Epidemiology & Disease Control Division and Policy, Research & Surveillance Group Ministry of Health and Health Promotion Board, Singapore. National Population Health Survey 2020. https://www.hpb.gov.sg/community/national-population-health-survey/survey-findings
[2] The Straits Times (14 Dec 2017). More than 1 in 3 newly diagnosed diabetics are not committed to taking their medication: Study. https://www.straitstimes.com/singapore/over-one-in-three-diabetics-not-committed-to-taking-their-medication-nhg-study
[3] The Straits Times (12 Aug 2022). Lose the weight - and the diabetes: S’pore healthcare group’s latest battle plan in war against disease https://www.straitstimes.com/singapore/health/lose-the-weight-and-the-diabetes-healthcare-groups-latest-battle-plan-in-war-against-disease
and
Clinical Trials.gov. Effectiveness of a weight management programme on diabetes remission in obese patients with early diabetes https://clinicaltrials.gov/study/NCT05762120?cond=NCT05762120&rank=1

